Medical Devices
A certificate of compliance with ISO-13485 (Medical Devices – Quality Management Systems – Requirements... View more
E/M Codes – Evaluation and Management Coding Documentation Guidelines
-
E/M Codes – Evaluation and Management Coding Documentation Guidelines
Evaluation and management coding (commonly known as E/M coding or E&M coding) is a medical coding process in support of medical billing. Practicing health care providers in the United States must use E/M coding to be reimbursed by Medicare, Medicaid programs, or private insurance for patient encounters. E/M coding is the process by which physician-patient encounters are translated into five digit CPT codes to facilitate billing.
E/M standards and guidelines were established by Congress in 1995 and revised in 1997. It has been adopted by private health insurance companies as the standard guidelines for determining type and severity of patient conditions. This allows medical service providers to document and bill for reimbursement for services provided. There are different E/M codes for different types of encounters such as office visits or hospital visits.
What are the E/M Guidelines?
The documentation requirements for each individual E/M code are dictated by a set of rules called the E/M guidelines. The E/M guidelines were developed by the Center for Medicare and Medicaid Services (CMS) in conjunction with the American Medical Association. Two versions have been released—the first in 1995 and the last in 1997.
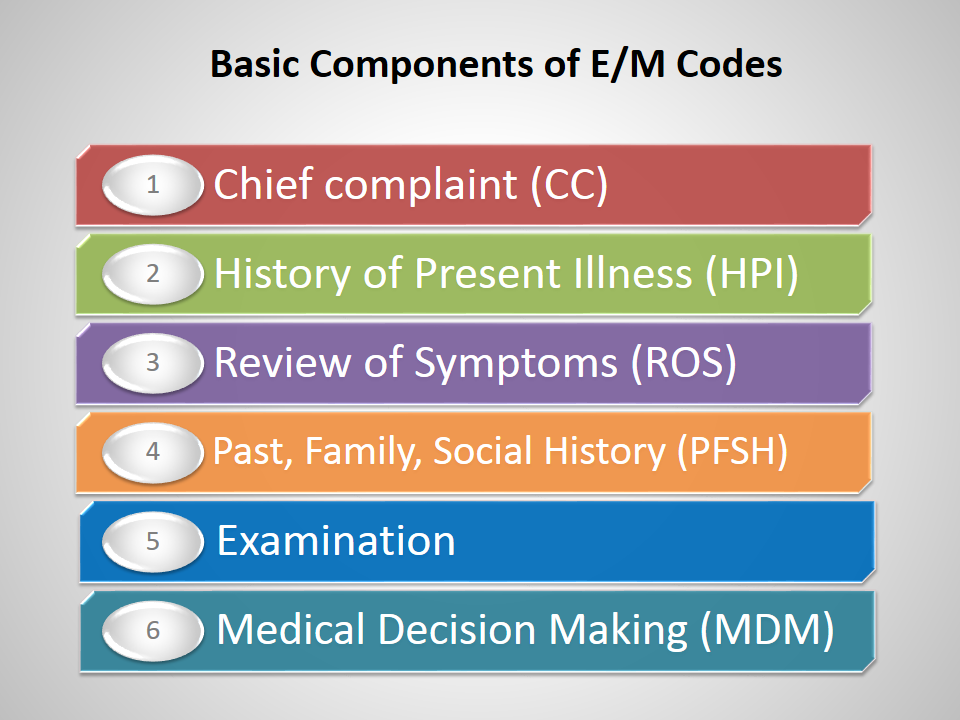
Components of E/M Codes
Chief complaint (CC) –
Purpose for the patient encounter, typically in the patient’s own words (e.g., patient complains of upset stomach)
History of Present Illness (HPI) –
- Description of the CC
- Location
- Duration
- Severity
- Context
- Quality
- Timing
- Modifying factors
- Associated signs and symptoms
Review of Symptoms (ROS) –
ROS is an inventory taken from the patient through questions for recognizing symptoms the patient currently has or has had in body systems. Systems include:
- Constitutional (e.g., vital signs, general appearance)
- Eyes
- Ears, nose, throat
- Cardiovascular
- Respiratory
- Gastrointestinal
- Genitourinary
- Musculoskeletal
- Integumentary (skin/breast)
- Neurological
- Psychiatric
- Endocrine
- Hematologic/Lymphatic
- Allergic/Immunologic
Past, Family, Social History (PFSH)
- Past – Previous illness, operations, injuries, and treatments
- Family – Family history that may place the patient at risk, including medical events, diseases, and hereditary conditions
- Social – Age appropriate review of patient activities (substance use, living arrangements, sexual history, employment, education, etc.)
Examination –
The levels of E/M services are based on four types of examinations:
- Problem Focused – Limited examination of the affected body area or organ system
- Expanded Problem Focused – Limited examination of the affected body area or organ system and any other symptomatic or related body area(s) or organ system(s)
- Detailed – Extended examination of the affected body area(s) or organ system(s) and any other symptomatic or related body area(s) or organ system(s)
- Comprehensive – General multi-system examination or complete examination of a single organ system
Medical Decision Making (MDM) –
Refers to the complexity of establishing a diagnosis and/or determining a management option. There are four levels of MDM in which selection is dependent upon the number of diagnoses, amount of data analyzed, and risk of complications.
- Straightforward
- Low complexity
- Moderate complexity
- High complexity
Sorry, there were no replies found.